In the years since the pandemic pushed virtual care into overdrive, one thing has become abundantly clear: telehealth is not a temporary fix, it’s a permanent pillar of modern clinical care. But not all telehealth setups are equal. Practices that used stand-alone video platforms quickly encountered multiple problems: double documentation, workflow fragmentation, loss of data continuity, and even compliance risk. The true win comes when virtual care is natively integrated into the EHR/clinical ecosystem: where scheduling, documentation, billing, and follow-ups all happen in one seamless workflow.
For physicians in primary care, specialists, small practices, or multi-site groups, the shift in 2025 is clear: the integrated EHR + telehealth platform is no longer “nice to have”, it’s a strategic operational necessity. Let’s explore the science, the stats, the workflow impacts, and how you as a clinician should evaluate telehealth in your practice.
Telehealth’s Evolution: From Crisis Response to Strategic Capability
-
The rapid growth
At the height of the COVID-19 pandemic, virtual visits surged. Some practices saw telehealth chalk up 30-40% of outpatient volume within weeks. Although levels settled afterward, data from FAIR Health in early 2025 show telehealth claims persist: in Q1 2025 ~14.9 % of patients in the U.S. had a telehealth claim in January, dropping slightly to ~14.5% by March. (fairhealth.org)
Globally, market analyses estimate the telehealth/telemedicine market will reach US $180+ billion by 2030, from ~US $94 billion in 2024. (GlobeNewswire)
For chronic-care, monitoring, and connectivity use-cases, one report projects telehealth-related home-care services for Medicare beneficiaries could reach ~US $265 billion by 2025. (thetechnotricks.net)
-
What changed
-
Regulatory flexibilities (e.g., via Centers for Medicare & Medicaid Services / CMS) made virtual visits reimbursable and originating-site rules looser.
-
Patients (especially younger and working-age) now expect virtual access. According to one dataset, age groups 19-30 and 31-40 accounted for nearly half of telehealth claimants in early 2025. (fairhealth.org)
-
Clinicians and practices realised that remote care can extend access (homebound, rural), reduce cancellations, and streamline workflow when done well.
Why Integrated Telehealth Matters for Physicians
-
Avoiding the “two-system” trap
Many clinics adopted video-only platforms tacked onto the side of their EHR. The problems:
-
Double data entry: manually copy video-visit notes into the EHR.
-
Documentation drift: virtual visit doesn’t auto-feed into the patient’s longitudinal chart.
-
Billing disconnect: reimbursement codes may be missed when virtual vs in-person workflows differ.
-
Fragmented reports: ePrescribe, orders, labs may originate outside the main system.
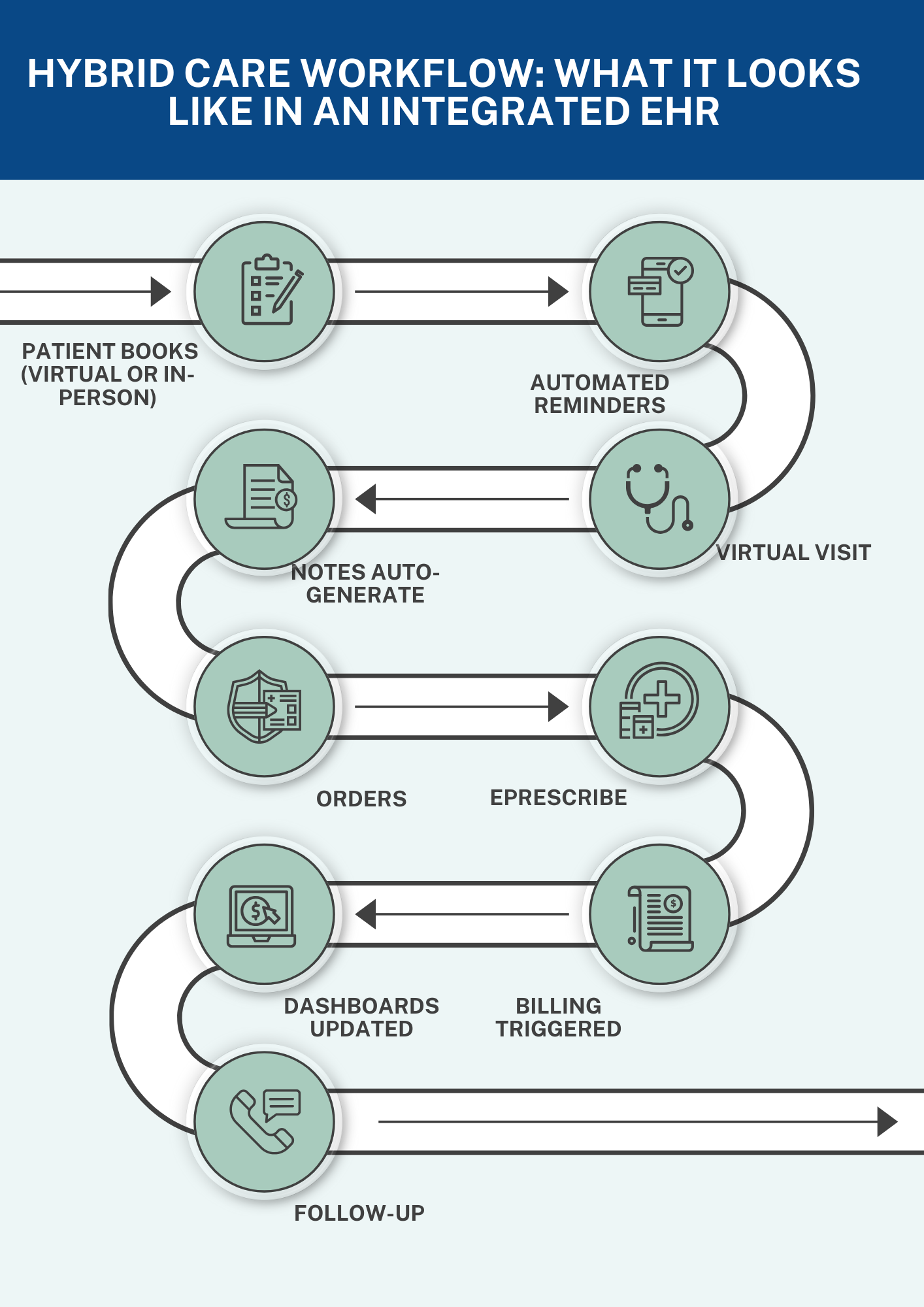
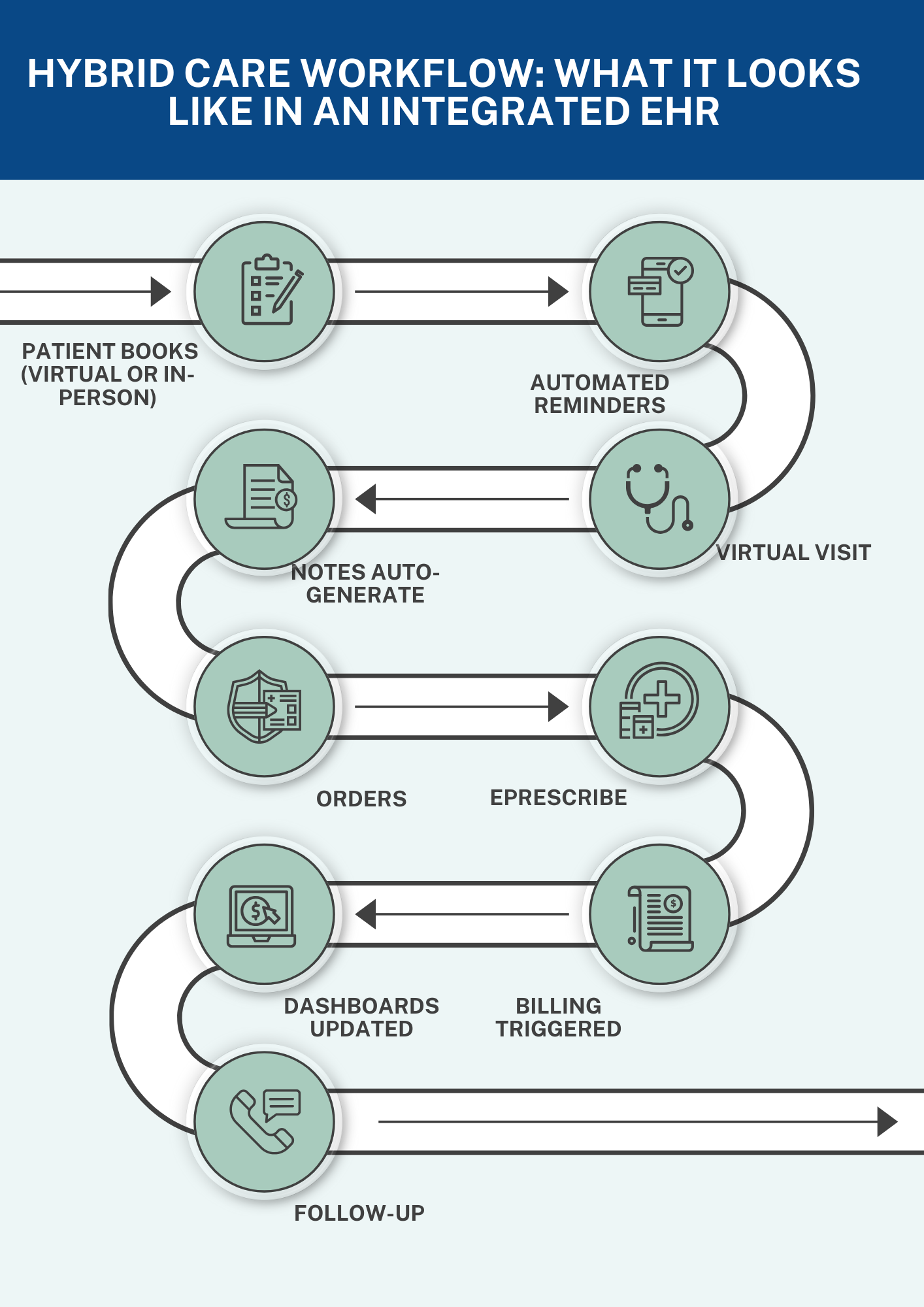
Integrated solutions (like those offered by MedTec) keep the virtual visit inside the same dashboard as the in-person visit: schedule → video start → chart opens → documentation auto-feeds → billing triggers. This reduces time, errors, and ensures continuity.
-
Clinical quality & patient experience
Research shows telehealth is not inferior to in-person care for a wide range of conditions—from mental health, follow-up care, chronic-disease check-ins, dermatology, and even acute triage. When the same EHR context is used for virtual visits, physicians are better positioned to:
-
Review prior labs/notes during the visit seamlessly.
-
Order tests or referrals on the spot.
-
Automate follow-ups and care-gap prompts.
-
Maintain compliance and documentation quality equivalent to in-office visits.
-
Operational benefits and practice efficiency
-
Higher convenience = fewer no-shows: patients skip travel, wait times, parking.
-
Expanded access: patients in rural/homebound settings.
-
Hybrid workflows: practices can schedule a mix of in-person + virtual visits.
-
Revenue opportunity: new visit types (tele-chronic care, remote monitoring) + better throughput.
-
Staff efficiency: front-desk and clinical teams don’t have to learn/use separate portals.
What the Data Tells Us (2025-Relevant Statistics for Clinicians)
-
Utilisation & patient demographic trends
-
Jan–Mar 2025: Telehealth claim share for patients dropped slightly from 14.9% → 14.5%. (fairhealth.org)
-
Telehealth remains significantly higher among 19-40 year-olds; lowest among 0-9 and 65+ in early-2025. (fairhealth.org)
-
Urban telehealth usage ~14.5% in March vs rural ~7.2%. (fairhealth.org)
-
Market size & growth forecasts
-
One analysis estimates telehealth market at US $148.04 billion in 2025, with a CAGR ~38.7% (2023-2030) driven by remote monitoring, AI, virtual consults. (TeleMedTrends)
-
Another report projects global era: ~US $1,044.92 billion by 2033. (precedenceresearch.com)
-
Technology adoption and hybrid models
-
More than 80% of patients and providers report preference for hybrid care (virtual + in-person) as of 2025. (Storm3)
-
Remote Patient Monitoring (RPM) devices (wearables, biosensors) are a major driver; they reduce readmissions, improve medication adherence in chronic disease. (TeleMedTrends)
-
Regulation, reimbursement & risk
-
Regulatory ‘policy cliff’ looms: permanent federal telehealth policy is still unresolved. (Storm3)
-
Employers and payers are increasingly embedding telehealth in benefits; e.g., by 2025 many employer plans cover virtual care broadly. (Taylor Benefits Insurance Agency)
How Practices (Small & Large) Can Leverage Integrated Telehealth + EHR
-
For small private practices
-
Choose a telehealth tool native to your EHR (or tightly integrated) so charting, scheduling, billing live in one system.
-
Set virtual-visit templates: include video, note auto-generation, ePrescribe, follow-up built-in.
-
Track no-show/cancellation rates for virtual vs in-person; many practices find virtual reduces the former.
-
Offer next-day/after-hours virtual check-ins to improve access.
-
For multi-site groups / MSOs
-
Standardize telehealth workflows across sites: one dashboard means consistent documentation, coding, compliance.
-
Use analytics to compare virtual vs in-person outcomes, cost, utilisation across specialties.
-
Build hybrid models: e.g., initial consult virtual → in-person procedure → virtual follow-up.
-
Leverage RPM (remote monitoring) for chronic disease hubs; integrate that data back into EHR and virtual visits.
-
For specialists
-
Tele-follow-ups: many specialties (cardiology, orthopedics, psychiatry, neurology) can reduce in-person burden via virtual check-ins.
-
Procedural/diagnostic patients: use virtual pre-visit to gather history, imaging review; in-person encounter for procedure.
-
Virtual multidisciplinary meetings: patients, surgeons, rehab teams via the same platform.
-
Ensure documentation captures complexity (e.g., remote-visit modifiers, care coordination codes); integrated EHR helps auto-flag these.
-
Training & workflow tips
-
Train staff: scheduling, front-desk, nursing triage—virtual workflow differs.
-
Pre-visit tech check: send patient instructions ahead (camera, microphone, privacy).
-
Use provider time appropriately: avoid switching platforms mid-visit.
-
After-visit process: orders, prescriptions, follow-up should trigger automatically from virtual encounter.
Why Integrated EHR + Telehealth Beats Stand-Alone Platforms
-
Single source of truth
Patient data lives in one system—virtual visit details, orders, prescriptions, follow-up tasks all tied to the same chart. Reduces risk of “visit outside the record.”
-
Billing and compliance alignment
When virtual and in-person care flow through the same system, documentation and billing codes (including modifiers, time-based codes) are more reliably captured and verified.
-
Better patient experience
Patients don’t need separate portals, log-ins, or different workflows for virtual vs in-office. When clinicians access their chart seamlessly, visit quality improves.
-
Data analytics & population health
With integrated telehealth, practices can monitor virtual visit outcomes, compare across modalities, track care gaps, apply predictive analytics. Multi-site groups especially benefit.
-
Future-proofing
Telehealth will evolve (AI triage, ambient video, RPM). An integrated EHR platform is already positioned for these advancements. Stand-alone tools may require re-platforming or data migration.
Clinical Use-Cases & Specialty Scenarios
Primary Care
-
Virtual chronic-disease check-in (diabetes, hypertension) with RPM device data streaming into the chart → clinician reviews during the virtual visit.
-
Behavioral health check-ins: often no imaging or lab required, so virtual improves access and continuity.
-
Preventive-care or vaccine counselling: virtual pre-visit, then schedule in-office for immunization.
Cardiology
-
Post-procedure follow-up (e.g., post-PCI) via telehealth with RPM (blood pressure, heart rate) reviewed.
-
Heart-failure monitoring: virtual visit + remote weight/BP tracking → early intervention.
-
Virtual ECG or echocardiogram review with patient and clinician discussing results together.
Orthopedics & Rehabilitation
-
Pre-operative virtual consultation: imaging reviewed, surgical discussion, consent process started.
-
Post-operative rehab check: patient uses wearable, sends biomechanics data, clinician assesses progress remotely.
-
Hybrid model: virtual PT check-in + in-person when major milestone reached.
Psychiatry / Behavioral Health
-
Virtual visits ideal—no travel barrier, more flexible scheduling.
-
Integrated EHR means notes, prescriptions, lab/care-gap tracking (e.g., metabolic labs for atypical antipsychotics) feed directly.
-
RPM of wellness metrics (sleep, activity) integrated into virtual check-in.
Key Risks & How to Mitigate Them
-
Regulatory & reimbursement risk
-
Telehealth policy remains in flux: the “policy cliff” for Medicare and state licencing still looms. (Storm3)
-
Ensure your platform supports virtual-visit modifiers, meets documentation standards, and can adapt with reimbursement changes.
-
Digital-divide & access equity
-
Rural populations still have lower telehealth uptake: early 2025 data shows ~7.2% of rural patients had a telehealth claim vs ~14.5% urban. (fairhealth.org)
-
Practices should support patients with technical education, choose platforms with low-bandwidth options, and leverage phone-only or asynchronous care where needed.
-
Data integration & security
-
Virtual tools generate more data (video, RPM, mobile health). EHR integration must ensure compliance, security, data-flow integrity.
-
Use platforms with end-to-end encryption and vendor-management oversight.
-
Clinical-workflow disruption
-
Virtual visits are not the same as in-person. Without workflow redesign, you risk incomplete data capture, missing exam elements, poor follow-up.
-
Define virtual-specific documentation checklists. Use templates optimized for virtual, train providers.
Putting It All Together: What Physicians Should Do Now
-
Audit your current telehealth setup:
-
Is it embedded in your EHR or a separate platform?
-
What is the no-show/cancel rate for virtual vs in-person?
-
How is billing and documentation managed for virtual visits?
-
Select an integrated telehealth/EHR platform if you haven’t already (or verify your current platform’s capabilities):
-
Scheduling, charting, e-prescribe, billing, and reporting in one workflow.
-
Support for RPM and hybrid care.
-
Data analytics for virtual vs in-office outcomes.
-
Compliance support: documentation, modifiers, licencing checks.
-
Define clinical workflows for hybrid care:
-
For each specialty/service line, decide which visits are virtual, which are in-person, and how follow-ups are managed.
-
Train staff and providers in virtual-visit best practices (pre-visit tech check, chart review, documentation template for virtual).
-
Measure performance:
-
Track patient satisfaction, no-show/cancel rate, visit volume, clinical outcomes, documentation/billing accuracy, physician time outside clinic.
-
Compare virtual vs in-person and adjust.
-
Explore RPM and remote monitoring:
-
For chronic diseases, integrate wearables/sensors so that virtual visits are enriched by data.
-
Leverage this data for early intervention, better outcomes, and increased value in hybrid care models.
-
Stay abreast of policy changes:
-
Reimbursement, licensure, originating site rules continue to evolve.
-
Work with your billing/compliance team to ensure your policy covers virtual visits, and documentation is audit-ready.