For more than a decade, clinicians have fought a losing battle against electronic documentation. Whether in primary care, specialty clinics, or multi-site medical groups, physicians consistently report that typing and navigating the EHR consume more mental energy than the clinical encounter itself.
And the data backs this up:
-
A 2024 national analysis found that physicians spend 5.8 hours per 8-hour clinic day inside the EHR—not including after-hours work.
-
Documentation alone averages 2.3 hours per day.
-
Across specialties, clinicians often spend 16–22 minutes of EHR time per patient, with documentation representing nearly one-quarter of that burden.
Typing and clicking have become the “silent comorbidities” of EHRs—undermining efficiency, increasing burnout, and shifting attention away from patients.
But in 2025, a major shift is underway: speech-to-text is emerging as the new default input method for clinical documentation. Modern systems—like MedTec’s integrated speech engine—go well beyond classical dictation. They use medical-grade NLP, specialty vocabularies, context recognition, and AI structuring to convert natural conversation into highly accurate, fully formatted clinical notes.
This blog examines the science, workflow impact, and practical clinical reasons why speech-to-text is rapidly becoming the standard for modern EHR documentation.
Why Typing Has Become Clinically Unsustainable
-
Cognitive fragmentation harms clinical performance
Typing during encounters creates cognitive switching costs—forcing clinicians to divide attention between listening, thinking, and documenting. Studies show that constant task-switching reduces diagnostic accuracy, impairs recall, and increases documentation omissions.
Primary care physicians now face an average of 130 EHR inbox messages per day across some systems. Hospitalists routinely have over 4,000 clicks per shift, according to time-motion studies. Specialists—particularly cardiologists, neurologists, and orthopedic surgeons—must document complex procedural or longitudinal details where structured templates fall short.
Typing is not just inefficient. It’s clinically risky.
-
The “pajama time” epidemic
More than 63% of physicians spend an hour or more each day finishing charts at home. Family medicine and internal medicine are the hardest hit.
Typing is a major contributor.
Physicians who rely on typing are far more likely to have incomplete notes, delayed sign-offs, and after-hours EHR tasks that spill into personal time. Burnout correlates strongly with time spent typing notes—not time spent seeing patients.
-
Typing encourages shorthand that reduces clarity
Typing pushes clinicians to abbreviate:
-
“Pt c/o CP x3d, worse w/ exertion, no SOB.”
-
“R knee OA, worsening; cont PT, RTC 3 mo.”
While shorthand is fast, it creates problems:
-
Billing teams struggle to justify E/M levels
-
Specialists lose key diagnostic details
-
Consultants receive vague summaries
-
Audits increase when MDM language is minimal
Speech-to-text reverses this problem by allowing natural, complete language.
Why Speech-to-Text Is the New Standard (Not Just a Convenience)
-
Clinicians speak 3–7× faster than they type
Average typing speed for physicians: 40–60 WPM (words per minute)
Average speaking speed: 120–160 WPM
Even with pauses, speech is by far the more efficient modality.
For specialties with verbose note requirements—psychiatry, cardiology, orthopedics, neurology—this difference is dramatic.
-
Speech captures natural clinical reasoning
Typing encourages short, fragmented documentation.
Speaking allows clinicians to articulate:
-
Differential reasoning
-
Rationale for diagnostic steps
-
Patient education statements
-
Risk/benefit discussions
-
MDM elements necessary for correct coding
Modern AI-powered speech systems like MedTec’s transform this spoken logic into structured, readable, defensible documentation.
-
Modern speech-to-text is highly accurate in medical contexts
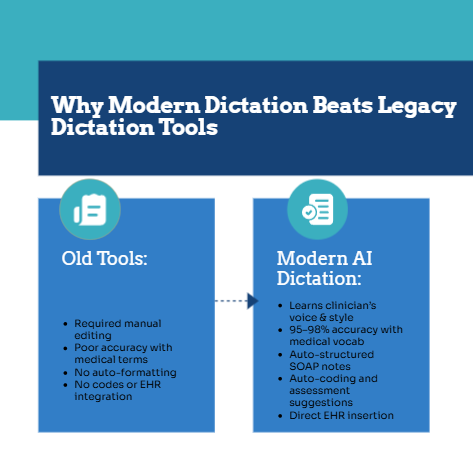
Older dictation tools struggled with:
-
Medication names
-
Laterality
-
Procedure terminology
-
Cross-specialty vocabulary
-
Abbreviations (“BID,” “PRN,” “NTG,” “A-fib”)
MedTec’s speech engine uses:
-
Medical language models trained across specialties
-
Acoustic models optimized for clinical environments
-
Semantic parsing that understands context
-
Automatic formatting into SOAP, A/P, and procedural structures
This increases accuracy and reduces the need for manual edits.
-
Reduces click fatigue and navigation burden
Physicians spend up to 33% of their EHR time on chart review and 24% on documentation (Annals of Internal Medicine, 2020). Many of these tasks involve:
-
Scrolling
-
Selecting templates
-
Expanding fields
-
Typing text into multiple boxes
-
Re-entering data already stated verbally during the visit
Speech-to-text removes many of these micro-tasks.
How MedTec’s Next-Generation Speech-to-Text Works (Clinician-Focused Overview)
MedTec’s implementation is not a standalone dictation tool. It’s an embedded clinical intelligence layer that operates within the EHR environment.
Here’s how physicians use it in practice:
Step 1: Speak naturally, not robotically
Providers can narrate in real time:
“The patient presents with chronic lower back pain, worsening over the past month. No red flag symptoms. Pain is aggravated by prolonged sitting…”
The system converts this into a fully formatted HPI.
Step 2: Automatic structuring
MedTec identifies semantic sections like:
-
HPI
-
ROS
-
Physical exam
-
Assessment
-
Plan
-
Orders
-
Follow-up instructions
Providers do not have to “tell” the system where to place information.
Step 3: Specialty-specific vocabulary recognition
Examples:
-
Cardiology: “NYHA II dyspnea,” “non-valvular AFib,” “LVEF 35%”
-
Psychiatry: “racing thoughts,” “avoidant behavior,” “SI/HI denied”
-
Orthopedics: “positive McMurray,” “ROM 10°–110°,” “valgus stress”
-
Neurology: “intermittent aura,” “unsteady tandem gait,” “pronator drift”
Specialists report dramatically fewer corrections.
Step 4: Automatic coding and compliance suggestions
Speech-to-text integrates with MedTec’s AI assistant to provide:
-
E/M level suggestions
-
Missing exam elements
-
Chronic condition updates
-
Appropriate follow-up timeframes
-
Procedure coding cues
Step 5: Edit minimally, sign confidently
Because the output is formatted cleanly and accurately, the review process is short.
Your Content Goes Here
Evidence: What Studies Show About Speech-to-Text and AI Aided Documentation
-
Time savings
Research on AI documentation tools (Medscape, JAMA, JMIR) shows:
-
30–70% reduction in documentation time
-
40–90 minutes saved per day
-
Fewer after-hours EHR sessions
-
Reduced cognitive workload
One recent multicenter study found:
-
47% of clinicians using an AI tool reported less time spent documenting at home
-
Compared to only 14.5% of clinicians in the control group
-
Increased documentation completeness
AI-assisted speech tools improve:
-
Chronic condition documentation
-
MDM clarity
-
HPI quality
-
Audit defense
-
E/M accuracy
A systematic review (Healthcare Journal, 2024) reported:
-
Documentation deficiency rates decreased from 8.6% to 6.3%
-
Notes were more thorough and clinically descriptive
-
Quality indices improved across specialties
-
Improved physician satisfaction and reduced burnout
Studies repeatedly show that clinicians feel:
-
Less exhausted
-
More in control
-
Less rushed during visits
-
More able to focus on patients
Speech-to-text restores conversational medicine.
Specialty-Specific Advantages
Primary Care
-
Rapid documentation for high-volume schedules
-
Better chronic condition tracking
-
Patient education easily verbalized
-
More complete social history and preventive care coverage
Cardiology
-
Accurate interpretation of functional classifications
-
Streamlined procedural dictations
-
Clear assessment of risk profiles
Orthopedics
-
Fast musculoskeletal exam documentation
-
Detailed injury mechanisms
-
Surgical planning notes captured more naturally
Psychiatry
-
Rich narrative detail (critical for medico-legal protection)
-
Medication adherence summaries
-
Full documentation of SI/HI discussions
Neurology
-
Nuanced symptom evolution
-
Gait, reflex, and sensory exam nuances
-
Differential reasoning captured without typing interruption
Speech-to-Text + AI Assistant: A Closed Loop of Efficiency
Speech-to-text alone is powerful.
But paired with MedTec’s AI medical assistant, clinicians get a complete workflow engine:
-
Real-time documentation
-
AI-identified gaps
-
Suggested diagnoses and codes
-
Formatted notes
-
Compliance checks
-
Auto-generated plans
-
Optional ambient listening for hands-free capture
This combination is what’s redefining documentation in modern practices.


